What is Obstetrics?
Singapore obstetrics focuses on the well-being of a woman during pregnancy, labour and delivery, and postpartum. The health of the foetus is also monitored closely to ensure optimal development. Obstetrics also covers preconception services, which include evaluating a woman’s fertility and treating certain gynaecological conditions that may affect her chances of pregnancy.
On top of routine screenings as the pregnancy progresses, obstetricians in Singapore also manage any complications that may arise during pregnancy or childbirth, such as gestational diabetes, preterm labour, or preeclampsia. Obstetricians are also skilled in both natural birth techniques as well as Caesarean section to ensure the safety of both mother and baby. Overall, obstetricians play a crucial role in helping women have healthy pregnancies and safe deliveries.
We know from scientific studies that babies born at the extremes of birthweight either under 2.5kg or over 4.5kg are at
an increased risk of developing chronic diseases later in life such as diabetes and heart disease. Studies have also
found that food chemicals can act to switch certain genes on and off in the developing fetus during pregnancy through a
process called ‘epigenetics’. A mother’s nutrition is therefore important even before she is pregnant as it can affect
the development and subsequent health of her baby.
Being overweight or underweight can also affect fertility. Hence, optimizing ones’ health and observing a healthy diet
and lifestyle should begin even before conception and pregnancy as it can affect a couple's chance of getting pregnant
in the first place.
If you have plans to start trying to conceive, consider making an appointment with us for a Prepregnancy or
Preconception health screen and consultation, where we can address your concerns, and discuss diet and lifestyle issues
for a healthy pregnancy.
What Does an Obstetrician Do?
An obstetrician in Singapore is a specialist doctor who helps with the safe and compassionate management of pregnancies and deliveries. Obstetric clinics should be well-equipped and licensed to ensure that services rendered are of high quality. It is recommended to visit an obstetrician if you are planning to conceive, as well as throughout the length of your pregnancy to ensure a safe and reassuring experience.
Pre-pregnancy Health Screen
Going for a pre-pregnancy health screening package is ideal to ensure that any health issues are addressed before
pregnancy. This usually comprises a thorough examination and investigations.
We will then review the investigation results and provide the necessary advice with regard to fertility and pregnancy.
For example, if a patient is found to lack immunity against rubella, vaccination is advisable as infection during
pregnancy can cause congenital defects in the baby.
Pregnancy Tests
Prenatal tests are performed throughout pregnancy. The exact tests ordered will depend on the stage of the pregnancy, the age and health of the mother, the medical history of both parents, and the family history. Ideally, mums-to-be should seek a consultation with their obstetrician & gynaecologist as soon as they are pregnant in order to allow the appropriate tests to be scheduled.
At every prenatal visit, an assessment of the mum-to-be’s weight, height, blood pressure and urine- analysis are performed. These help to screen for any high blood pressure, infections or gestational diabetes. In many cases, complications can be avoided if early diagnosis is made and treatment initiated.
- Maternal full blood count for screening for anaemia, sickle cell disease and thalassaemia. If necessary, paternal blood testing is undertaken so that the probability of the fetus being affected can be assessed.
- Maternal blood group and RhD status to screen for haemolytic disease of the newborn. All non-sensitised pregnant women who are RhD-negative are offered routine antenatal anti-D prophylaxis.
- Screening for hepatitis B, HIV and syphilis. This means that effective postnatal intervention can be offered to infected women to decrease the risk of mother-to-child transmission.
- Screening for rubella (German measles) immunity. If a woman is found to not have immunity, it will be recommended that she avoid contact with infected individuals during her pregnancy and receive a vaccination against rubella after she gives birth
Pregnancy Screening
 This test is also known as the OSCAR (One-Stop Clinic for Assessment of Risks of Fetal Anomalies).
This includes a scan of the nuchal translucency or fluid-filled space behind the fetal neck. A nasal bone assessment is
also usually done as babies with Down’s Syndrome may have an absence of the nasal bone.
The scans may be combined with a blood test from the mother for hormone and biochemical markers for
a more accurate risk assessment.
This test is also known as the OSCAR (One-Stop Clinic for Assessment of Risks of Fetal Anomalies).
This includes a scan of the nuchal translucency or fluid-filled space behind the fetal neck. A nasal bone assessment is
also usually done as babies with Down’s Syndrome may have an absence of the nasal bone.
The scans may be combined with a blood test from the mother for hormone and biochemical markers for
a more accurate risk assessment.
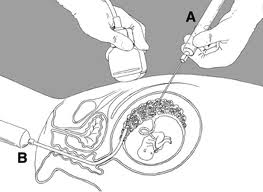
The CVS can be carried out earlier - usually between 10-13 weeks of pregnancy. It involves sampling of the developing placenta and again the same type of analysis of fetal cells to detect chromosomal, genetically inherited and endocrine or metabolic conditions can be performed. There is a risk of miscarriage of 1-2%. While these diagnostic tests help to confirm if the baby truly carries a chromosomal disorder, these tests are invasive and carry a small risk of miscarriage. Hence, they are not offered as a routine.

Pregnancy Scanning and Pregnancy Care Singapore
 A 3D scan provides a life-like image of your baby while a 4D scan is a real-time moving image of the baby. These scans
may take around 30 minutes or longer depending on your baby’s position and movement.
They may help to provide reassurance that the baby is growing well, but are not meant to replace the screening scans which
are advised in the second trimester.
A 3D scan provides a life-like image of your baby while a 4D scan is a real-time moving image of the baby. These scans
may take around 30 minutes or longer depending on your baby’s position and movement.
They may help to provide reassurance that the baby is growing well, but are not meant to replace the screening scans which
are advised in the second trimester.
Delivery and Postnatal Care
 The 3 modes of delivery are normal vaginal delivery, assisted or instrumental delivery, and Caesarean. Most women are
encouraged to try for a normal vaginal delivery. Occasionally, some require help with forceps or a vacuum cup. Others
may require a Caesarean section.
The 3 modes of delivery are normal vaginal delivery, assisted or instrumental delivery, and Caesarean. Most women are
encouraged to try for a normal vaginal delivery. Occasionally, some require help with forceps or a vacuum cup. Others
may require a Caesarean section.
Each mode of delivery has its benefits and risks. Every woman is unique with different pain thresholds and perceptions of how their delivery should be conducted. Do share with us your birth plan so that we can work with you towards the safe delivery of your child.


Dr Loi is a firm believer of providing compassionate and comprehensive care for her pregnant and postpartum patients, allowing them to make informed decisions and gain access to high-quality, personalised treatments. Today, she is the Medical Director of the Health & Fertility Centre for Women and Monash IVF Singapore; and continues to contribute actively to the advancement of the field of reproductive health through research and teaching.
Mount Elizabeth Medical Centre
Singapore 228510
